Understanding how hepatologists diagnose liver problems is crucial for anyone experiencing symptoms such as fatigue, abdominal discomfort, jaundice, dark urine, or unexplained weight fluctuations. The liver is a vital organ responsible for detoxification, metabolism, and maintaining overall health. Subtle changes in liver function can indicate serious conditions like hepatitis, fatty liver disease, cirrhosis, or liver cancer. Many liver disorders develop silently, which makes early evaluation by a specialist essential to prevent progression and ensure effective management.
Hepatologists combine comprehensive medical history, physical examinations, laboratory testing, advanced imaging, and specialized procedures to identify underlying causes, determine disease severity, and formulate personalized treatment plans. Patients in regions such as Kochi, Kerala, and Sharjah are increasingly seeking professional guidance, recognizing that early diagnosis improves outcomes, enhances quality of life, and supports long-term liver wellness. This article explores the diagnostic journey, highlighting key tests, procedures, and strategies used by liver specialists to maintain optimal liver health.
Comprehensive Clinical Evaluation
The diagnostic journey begins with a thorough clinical evaluation. Hepatologists gather information about:
-
Medical history: Past liver conditions, medications, alcohol consumption, viral infections
-
Family history: Genetic liver disorders or autoimmune conditions
-
Lifestyle factors: Diet, physical activity, alcohol or drug use
During the physical examination, specialists look for jaundice, liver enlargement, abdominal swelling, and signs of chronic liver disease such as spider angiomas or palmar erythema. This stage provides a crucial foundation for determining which tests and procedures are necessary, ensuring a tailored and effective diagnostic approach.
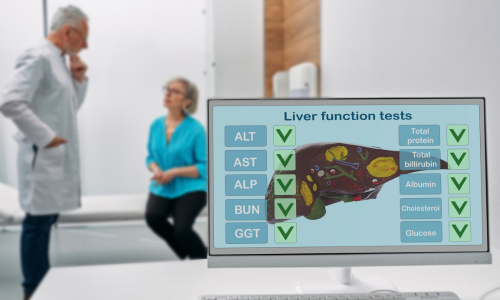
Laboratory Testing: Key Insights into Liver Function
Laboratory investigations are central to evaluating liver health. They help identify conditions ranging from fatty liver and hepatitis to cirrhosis and early liver cancer.
Liver Function Tests (LFTs) measure enzymes, proteins, and bilirubin levels to detect inflammation or liver cell damage. Common markers include ALT, AST, ALP, GGT, albumin, and bilirubin.
Viral Hepatitis Screening is essential to detect hepatitis A, B, or C infections, guiding timely antiviral therapy.
Metabolic and Autoimmune Panels evaluate disorders such as autoimmune hepatitis, hemochromatosis, or Wilson’s disease.
Complete Blood Count (CBC) and Coagulation Tests assess overall health and identify complications related to chronic liver disease, such as anemia or clotting abnormalities.
Laboratory tests provide critical insights that guide imaging studies and advanced procedures, ensuring that hepatologists can accurately pinpoint the nature and severity of liver issues.
Imaging Techniques: Visualizing Liver Structure
Imaging allows hepatologists to assess the liver’s structure, detect abnormalities, and monitor disease progression.
Ultrasound (USG) is commonly used to evaluate liver size, texture, fatty infiltration, fibrosis, cysts, or tumors.
Computed Tomography (CT) Scan provides detailed 3D images, helping identify structural changes or vascular complications.
Magnetic Resonance Imaging (MRI) and MRCP offer high-resolution views of liver tissue and bile ducts, aiding in complex diagnoses.
Elastography (FibroScan) measures liver stiffness, evaluating fibrosis or cirrhosis without the need for invasive procedures.
Imaging complements lab tests by giving hepatologists a visual understanding of liver health and guiding treatment decisions.
Specialized Procedures
Some liver conditions require targeted procedures for precise diagnosis:
Liver Biopsy involves removing a small tissue sample to examine inflammation, fibrosis, or early signs of liver cancer. This minimally invasive procedure provides definitive insights into liver health.
Endoscopic Procedures (ERCP) are used to evaluate and treat bile duct disorders, allowing direct assessment and sometimes therapeutic intervention.
Genetic and Metabolic Testing identifies rare liver disorders such as Wilson’s disease or alpha-1 antitrypsin deficiency, helping tailor personalized management strategies.
Emerging Non-Invasive and AI-Based Diagnostics
Modern hepatology is incorporating non-invasive methods and technology to enhance early detection and monitoring:
-
Non-Invasive Biomarkers include blood-based fibrosis scores like APRI or FibroTest, providing valuable information without tissue sampling.
-
Artificial Intelligence (AI) and Machine Learning assist in interpreting imaging results, predicting fibrosis progression, and supporting early intervention strategies.
These innovations complement traditional diagnostic methods, improving accuracy and patient experience while reinforcing the authority of hepatology care.
Lifestyle Factors and Risk Assessment
Understanding lifestyle and risk factors is critical for early detection and prevention:
-
Obesity, diabetes, and high cholesterol increase the risk of fatty liver disease.
-
Chronic viral infections, prolonged alcohol use, and certain medications contribute to liver damage.
-
Family history may indicate genetic susceptibility.
Patients are advised to maintain a balanced diet, regular physical activity, alcohol moderation, and routine monitoring to protect liver health.
Importance of Early Detection and Follow-Up
Proactive monitoring allows hepatologists to intervene early, reducing the risk of complications. Follow-up schedules are tailored based on risk factors, previous diagnoses, and the results of laboratory and imaging tests. Early detection supports lifestyle modifications, medication management, and timely therapeutic interventions, ultimately improving long-term outcomes.
Patient Education and Preparing for Tests
Patients play a key role in successful diagnosis:
-
Blood tests may require fasting or temporary medication adjustments.
-
Imaging procedures often require preparation such as wearing comfortable clothing or avoiding metal objects.
-
Biopsy procedures involve understanding the process, post-procedure care, and possible minor side effects.
Clear communication with hepatologists ensures accurate testing and reduces patient anxiety during evaluation.
Frequently Asked Questions
How can hepatologists detect liver problems early?
Early detection combines clinical evaluation, lab tests, imaging, and risk assessment to identify issues before severe symptoms develop.
Are liver tests painful or risky?
Most tests are non-invasive and safe. Procedures like liver biopsy may involve minor discomfort but are carefully managed.
Can lifestyle changes improve liver health?
Yes, especially in cases like fatty liver. Balanced nutrition, regular exercise, and limiting alcohol consumption can significantly improve liver function.
How often should liver health be monitored?
High-risk individuals may require more frequent evaluations, while healthy adults should consider annual check-ups or as advised by a hepatologist.
Is AI used in liver diagnostics?
Yes, AI helps analyze imaging results, predict disease progression, and support early intervention.
Conclusion
Understanding how hepatologists diagnose liver problems empowers patients to seek timely care, make informed decisions, and adopt preventive practices. From initial clinical evaluation and laboratory testing to imaging, specialized procedures, and emerging AI tools, liver specialists use a comprehensive approach to ensure accurate diagnosis and effective management. Patients in Kochi, Kerala, Sharjah, and across the UAE benefit from this structured, expert-guided process, enabling early intervention, lifestyle adjustments, and long-term liver wellness.