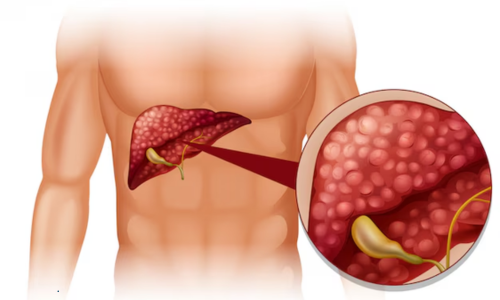
Cirrhosis is a serious liver condition that develops gradually over time, often without obvious symptoms in its early stages. It occurs when healthy liver tissue is replaced by scar tissue, affecting the liver’s ability to function properly. Understanding cirrhosis—its causes, stages, symptoms, and modern treatment options—is essential for early detection, effective management, and improved long-term outcomes.
This guide explains cirrhosis in a clear, patient-friendly way while covering the latest medical approaches used in modern liver care.
What Is Cirrhosis?
Cirrhosis is the result of long-term, continuous damage to the liver. As the liver attempts to repair itself, scar tissue forms. Over time, excessive scarring disrupts normal liver structure and blood flow, reducing the organ’s ability to perform essential functions such as:
-
Detoxifying harmful substances
-
Producing bile for digestion
-
Regulating blood clotting
-
Storing nutrients and energy
Cirrhosis is usually irreversible, but early diagnosis and proper treatment can slow progression and prevent complications.
Common Causes of Cirrhosis
Cirrhosis does not develop overnight. It is typically the end result of chronic liver disease. The most common causes include:
1. Chronic Alcohol Use
Long-term excessive alcohol consumption is a leading cause of cirrhosis. Alcohol damages liver cells and promotes inflammation and scarring.
2. Chronic Viral Hepatitis
-
Hepatitis B
-
Hepatitis C
Untreated viral hepatitis can cause ongoing liver inflammation, eventually leading to cirrhosis.
3. Non-Alcoholic Fatty Liver Disease (NAFLD)
Closely linked to obesity, diabetes, and metabolic syndrome, NAFLD can progress to non-alcoholic steatohepatitis (NASH), which may result in cirrhosis.
4. Autoimmune Liver Diseases
Conditions such as autoimmune hepatitis cause the immune system to attack liver cells, leading to chronic inflammation and scarring.
5. Genetic and Metabolic Disorders
Examples include:
-
Hemochromatosis (iron overload)
-
Wilson’s disease (copper accumulation)
6. Bile Duct Disorders
Diseases like primary biliary cholangitis or primary sclerosing cholangitis interfere with bile flow and damage liver tissue over time.
Stages of Cirrhosis
Cirrhosis progresses through distinct stages, each with different symptoms and treatment goals.
Stage 1: Compensated Cirrhosis
At this stage, the liver is scarred but still able to perform most of its functions.
Common features:
-
Few or no symptoms
-
Often detected through blood tests or imaging
-
Disease progression can be slowed with proper care
Stage 2: Decompensated Cirrhosis
As liver function declines, complications begin to appear.
Possible symptoms include:
-
Fatigue and weakness
-
Jaundice (yellowing of skin and eyes)
-
Fluid accumulation in the abdomen (ascites)
-
Swelling of legs and ankles
This stage requires close medical monitoring.
Stage 3: Advanced Decompensation
Complications become more severe and may include:
-
Variceal bleeding (enlarged veins in the esophagus)
-
Hepatic encephalopathy (confusion due to toxin buildup)
-
Frequent infections
Quality of life may be significantly affected at this stage.
Stage 4: End-Stage Liver Disease
At this stage, the liver can no longer sustain essential functions.
-
Severe complications are common
-
Liver transplantation may be considered for eligible patients
Symptoms of Cirrhosis
Symptoms vary depending on disease stage and cause. Early cirrhosis may be silent, while advanced stages show clear signs.
Common symptoms include:
-
Persistent fatigue
-
Loss of appetite and weight loss
-
Nausea
-
Itching
-
Easy bruising or bleeding
-
Mental confusion or memory issues
Early recognition of symptoms can significantly improve outcomes.
How Cirrhosis Is Diagnosed
Diagnosis usually involves a combination of clinical evaluation and investigations:
-
Blood tests: Liver function tests, clotting profile
-
Imaging: Ultrasound, CT scan, or MRI
-
Elastography: Measures liver stiffness
-
Liver biopsy: In selected cases to assess severity
Accurate staging is essential for planning appropriate treatment.
Modern Treatment Options for Cirrhosis
While cirrhosis-related scarring is often irreversible, modern treatments focus on slowing progression, managing complications, and improving quality of life.
1. Treating the Underlying Cause
This is the most important step.
-
Antiviral therapy for hepatitis B or C
-
Complete alcohol abstinence in alcohol-related cirrhosis
-
Weight management and metabolic control for fatty liver disease
Addressing the root cause can significantly slow liver damage.
2. Medications to Manage Symptoms and Complications
Depending on individual needs, doctors may prescribe:
-
Diuretics for fluid retention
-
Medications to reduce portal hypertension
-
Lactulose or rifaximin for hepatic encephalopathy
-
Vitamin and nutritional supplements
Treatment is personalized and closely monitored.
3. Lifestyle and Dietary Management
Lifestyle changes play a major role in managing cirrhosis safely:
-
Balanced, protein-adequate diet
-
Reduced salt intake for fluid control
-
Avoiding alcohol completely
-
Vaccination against hepatitis A and B
Medical nutrition therapy is often recommended.
4. Endoscopic and Interventional Procedures
For certain complications:
-
Endoscopic band ligation for varices
-
Paracentesis for severe ascites
-
TIPS (Transjugular Intrahepatic Portosystemic Shunt) in selected cases
These procedures help control life-threatening complications.
5. Liver Transplantation
For advanced cirrhosis or liver failure, transplantation may be considered.
-
Requires thorough evaluation
-
Strict eligibility criteria
-
Offers the possibility of long-term survival
Modern transplant medicine has significantly improved success rates.
Can Cirrhosis Be Prevented?
In many cases, yes.
Prevention strategies include:
-
Early treatment of hepatitis
-
Avoiding excessive alcohol consumption
-
Managing diabetes, obesity, and cholesterol
-
Regular liver check-ups for high-risk individuals
Early intervention is key to preventing irreversible damage.
Living with Cirrhosis: Long-Term Outlook
Living with cirrhosis requires ongoing care, but many people maintain a good quality of life with proper management.
Key factors that improve outcomes:
-
Early diagnosis
-
Regular follow-ups with a liver specialist
-
Adherence to treatment and lifestyle recommendations
Education and proactive care empower patients to manage the condition effectively.
Final Thoughts
Cirrhosis is a complex but manageable condition when identified early and treated appropriately. Understanding its causes, recognizing symptoms, and following modern medical treatment strategies can significantly slow disease progression and reduce complications.
With advances in hepatology, antiviral therapy, interventional procedures, and transplantation, patients today have more options than ever before. If liver disease is suspected, timely medical evaluation can make a life-changing difference.
FAQs on Cirrhosis
Q1: What is cirrhosis of the liver?
Cirrhosis is a chronic condition where healthy liver tissue is gradually replaced by scar tissue, reducing the liver’s ability to function properly. It usually develops over years due to long-term liver damage from causes such as hepatitis, alcohol use, or fatty liver disease.
Q2: What are the main causes of cirrhosis?
The most common causes of cirrhosis include chronic alcohol use, hepatitis B or C infection, non-alcoholic fatty liver disease, autoimmune liver disorders, and genetic conditions such as hemochromatosis or Wilson’s disease.
Q3: What are the early signs of cirrhosis?
Early cirrhosis may not cause noticeable symptoms. When present, early signs can include fatigue, mild abdominal discomfort, loss of appetite, and abnormal liver blood test results. Many cases are detected during routine health evaluations.
Q4: What are the stages of cirrhosis?
Cirrhosis progresses from compensated cirrhosis, where the liver still functions adequately, to decompensated cirrhosis, which involves complications such as ascites, jaundice, bleeding, and mental confusion. Advanced stages may lead to liver failure.
Q5: Can cirrhosis be reversed?
In most cases, cirrhosis-related scarring is not reversible. However, treating the underlying cause early can slow or stop disease progression and improve liver function. In advanced cases, liver transplantation may be considered.
Q6: How is cirrhosis diagnosed?
Cirrhosis is diagnosed using a combination of blood tests, imaging studies such as ultrasound or MRI, elastography to measure liver stiffness, and sometimes a liver biopsy to assess the extent of scarring.
Q7: What are the modern treatment options for cirrhosis?
Modern treatment focuses on managing the cause, preventing complications, and supporting liver function. This may include antiviral therapy, lifestyle modifications, medications, endoscopic procedures, and in advanced cases, liver transplantation.
Q8: Is cirrhosis life-threatening?
Cirrhosis can become life-threatening if complications develop, such as internal bleeding, severe infections, or liver failure. Early diagnosis, regular monitoring, and appropriate treatment can significantly improve survival and quality of life.
Q9: What lifestyle changes help manage cirrhosis?
Key lifestyle measures include avoiding alcohol completely, following a balanced low-sodium diet, maintaining a healthy weight, managing diabetes or cholesterol, and attending regular follow-up appointments with a liver specialist.
Q10: When should someone with cirrhosis see a specialist?
Anyone diagnosed with cirrhosis should be under the care of a gastroenterologist or hepatologist. Immediate medical attention is needed if symptoms such as jaundice, abdominal swelling, confusion, or vomiting blood occur.